
Repealing Essential Health Benefits Will Leave People with Preexisting Conditions Unprotected
03.09.2018
Members of Congress and the Trump Administration have frequently proposed measures that would eliminate or undermine essential health benefits (EHBs). One of the most popular aspects of the Affordable Care Act is its requirement that all individual and small group health plans (for people who don’t have traditional job-based coverage) cover these essential health benefits, which include maternity, mental health, preventive, and pediatric dental care.
The latest administrative threats come in the form of two proposed rules: One proposal would allow short-term health plans to be sold for long periods of time. These short-term policies do not have to cover essential health benefits. The second proposal would allow the sale of Association Health Plans (AHPs) to individuals, and association health plans would not have to cover essential health benefits. Other proposals that frequently arise allow states to weaken or waive essential health benefits.
This means getting rid of a core protection for people with preexisting conditions. And it would have devastating consequences for millions of people.
Weakening or eliminating EHB requirements would leave millions without any affordable health care options, forcing them to pay out of pocket for needed care or go without care all together.
What are Essential Health Benefits and why do they matter?
EHB requirements ensure that everyone in the individual and small group health insurance markets has access to comprehensive coverage that actually covers the services they need. Learn more about the 10 categories of benefits the Affordable Care Act requires all health plans to cover.
Because of EHB requirements, people with mental health or substance abuse disorders have the peace of mind of knowing that their plan must cover their needsand that their coverage for these mental health services must be as comprehensive as their coverage for medical and surgical services. Women can rest assured knowing that they will have maternity coverage when they become pregnant. People with developmental and intellectual disorders, like autism, benefit from habilitative services that help them learn, keep, or improve functional skills that help them achieve their personal ambitions. Millions of people have benefited from gaining coverage from these essential services under the ACA.
What would happen if the Essential Health Benefits are not required?
The nonpartisan Congressional Budget Office’s (CBO) analysis of the 2017 House of Representatives bill repealing the ACA shows the impact of allowing states to eliminate or weaken the essential health benefits. Half of people in this country live in states that would significantly weaken or eliminate their Essential Health Benefits.
CBO estimates that 1 in 3 people live in states that would opt to remove certain benefits from its EHB that were typically not covered before the ACA, like maternity care, rehabilitative and habiliative care and mental health/substance use treatment. Another 1 in 6 people live in states that would make more aggressive changes, even eliminating the essential health benefits completely.
In these states, plans would become very skimpy and once again discriminate against people with preexisting conditions. Without a requirement to cover some or all of the essential health benefits, CBO forecasts that two things would happen: 1) most insurers would stop offering comprehensive plans that include newly optional services, out of fear of attracting people with high health care needs; and 2) the few plans with coverage for services that are no longer required, like maternity care, mental health and substance use treatment, habilitative treatment, would likely only cover these services through expensive riders that increase premiums by as much as $1,000 each month.
In either of these scenarios, out-of-pocket health care costs would increase drastically for people with health conditions that required treatment no longer covered under the essential health benefits.
While on paper there might still be a ban on insurers discriminating against people with preexisting conditions, in practice, insurers would be discriminating against people with chronic conditions left and right. Not selling comprehensive coverage or making that coverage exorbitantly more expensive than plans that only cater to the needs of people in perfect health is discrimination against people with pre-existing conditions.
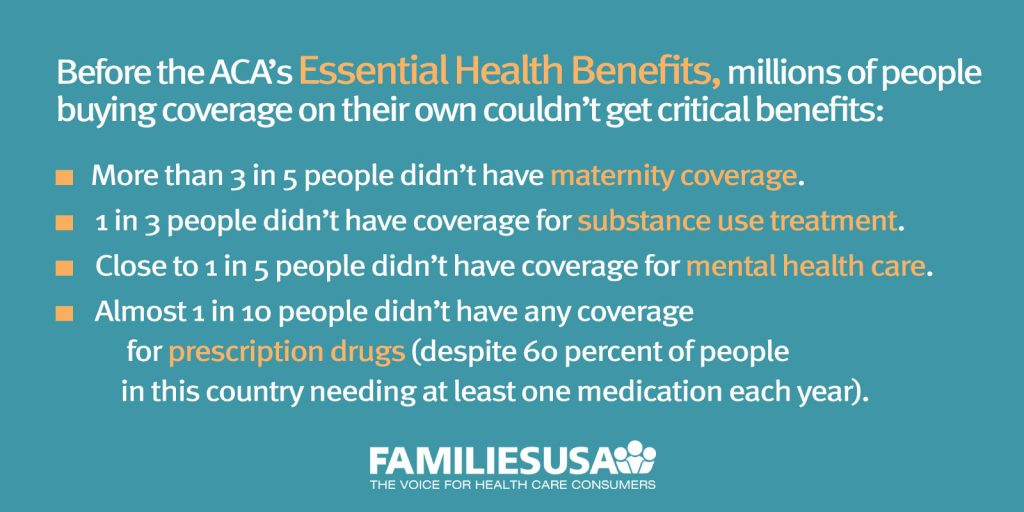
In total, it would be a return to the days before the ACA where it was it nearly impossible for people to find affordable coverage that actually covered their health care needs. Before these essential health benefits were in place, millions of people purchasing coverage on their own couldn’t get coverage for critical care:
- More than 3 in 5 people didn’t have maternity coverage.
- 1 in 3 people didn’t have coverage for substance use treatment.
- Close to 1 in 5 people didn’t have coverage for mental health care.
- Almost 1 in 10 people didn’t have any coverage for prescription drugs (despite 60 percent of people in this country needing at least one medication each year).
Caps on how much people have to pay out-of-pocket would vanish. The ACA placed a limit on the maximum amount of money anyone has to pay out of their own pocket for care in one year, called an out-of-pocket maximum. This year, the protective cap ensures that people with serious medical problems never have to pay more than $7,350 in a year for covered care, and families never have to pay more than $14,700.
This protection only applies to covered essential health benefits. If the essential health benefits goes away, so does this vital financial protection. This means that anyone purchasing a plan in the individual market would no longer be protected from exorbitant out-of-pocket costs and insurers could offer plans with extremely high deductibles and cost-sharing (e.g., copayments, coinsurance) – shifting more of the cost of care to consumers.
What would a plan look like without the Essential Health Benefits?
To get a better idea of what plans would and would not cover if essential benefit requirements went away, we looked at some top selling short-term health insurance policies sold in a number of states – policies that, under current rules, you can buy for up to 3 months and that do not have to follow the ACA.
Here’s what these plans commonly DO NOT cover:
- outpatient prescription drugs
- no mental health or substance use services
- no prenatal care or delivery services
- limited or no well-baby care
Several plans limited coverage for emergency room visits unless they resulted in an admission. They also covered barely any preventive care.
While those exclusions were advertised to shoppers through plan comparison tools, shoppers would have to read the fine print to see other dangerous exclusions hidden in small print, such as:
- No coverage for physical, speech, or occupational therapy
- No treatment for injuries from sports
- No treatment for self-inflicted injury or sickness
- Exclusions for orthopedic treatment
- No treatment for any congenital condition
- Six-month wait before certain procedures, like tonsillectomies
- No treatment for chronic pain, AIDS, or immunodeficiency orders
- No treatment for kidney or end-stage renal disease
- No treatment or diagnosis for allergies
- No treatment for joint replacement (unless related to a covered injury)
- No services or supplies for smoking cessation
- No organ or tissue transplants
- No weight loss/obesity treatment or surgery
- No treatment for acne or moles
At the end of the day, the equation is simple: Do we want a health care system that guarantees that every woman is able to afford maternity coverage when she is pregnant, that every child with a development disability is able to afford the therapy they need to fulfill their dreams, that every person struggling with addiction, like opioid use, can get the treatment they need, and that every person with a chronic condition is protected against discrimination? If so, we need the essential health benefits.
