HOW TO MAKE A HIGH-VALUE
HEALTH CARE SYSTEM
Here’s the good news. We already know how to start making things better. We just need to work together to make sure policymakers have the political will to make real and lasting changes.
Consumer health leaders must join with health care professionals, labor unions, employers, and others to counterbalance the entrenched business interests within the health care industry that drive predatory and abusive practices that drive up health care prices and result in unaffordable, low-quality care for our nation’s families and children, workers, and employers. And America’s leaders must come together and finally fix the problem once and for all.
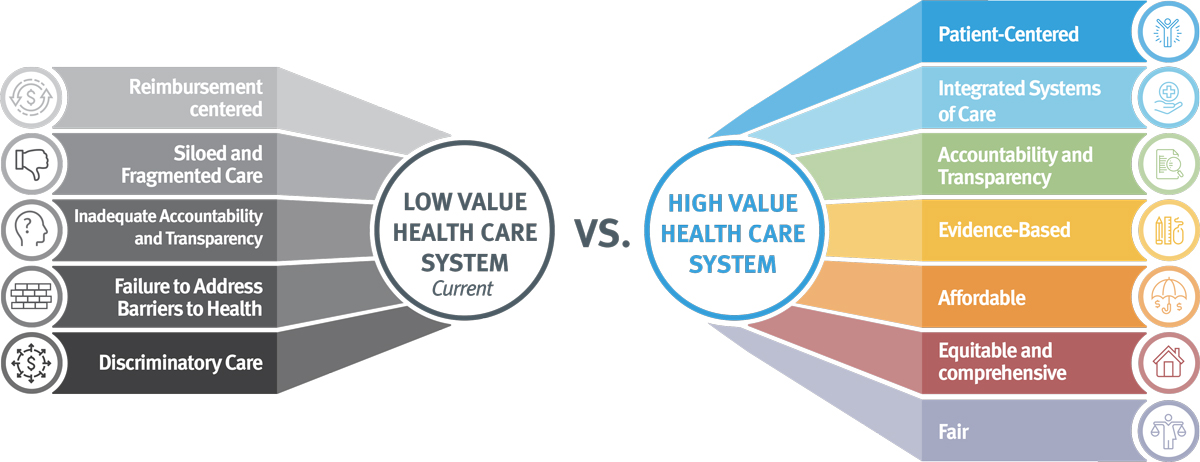
Reimbursement centered: costs and care delivery are driven by revenue-maximizing rather than patient outcomes
Siloed and Fragmented Care: lack of integrated and coordinated care leads to bad outcomes.
Inadequate Accountability and Transparency: lack of a national system that holds plans and providers accountable for low quality, poor outcomes, and the cost of health care, in a way that is transparent to the public
Failure to Address Barriers to Health: insufficient resources to address the effects of the social determinants of health on health outcomes and costs.
Discriminatory Care: Clinical interactions that treat people inadequately based on individual characteristics such as race, ethnicity, disability, or gender identity. High prices but low-quality care.
Patient-centered: care is driven by shared decision-making between the provider team and the individual’s preferences, needs, and values.
Integrated Systems of Care: health care payment and delivery are coordinated across all aspects of health including physical, behavioral, oral with strong primary care foundation.
Accountability and Transparency: the health care system is held accountable for the cost and quality of care, and the health of families in a transparent way to the public.
Evidence-Based: care is safe, effective, patient-centered, timely, efficient, and equitable.
Affordable: health care prices are competitive.
Equitable and Comprehensive: the system is equipped with the tools and resources needed to address the impact of the social determinants of health on health outcomes and costs.
Fair: care delivery is not distorted by a clinician or systemic bias.
 KEY WAYS WE CAN FIX THIS BROKEN SYSTEM
KEY WAYS WE CAN FIX THIS BROKEN SYSTEM
Drive down costs for consumers, working people, and employers by addressing consolidated health care markets.
One of the most notable predatory practices driving health care costs and high prices is increased consolidation of physician groups, hospitals, pharmaceutical companies, and insurance companies. Over the last decade, players in the health care industry have accumulated more power through mergers and acquisitions, strengthening their ability to increase health care prices without providing meaningful improvements in the health of the populations they serve.
This increased economic power also allows the health care industry to influence policy decisions that too often overlook the interests of families and shifts the burden of rising health care costs to families.
Critical to lowering health care costs is addressing consolidated health care markets by restoring market competition and increasing antitrust enforcement in the health care sector.
Lower prescription drug costs for our nation’s families.
In 2015, the United States spent $457 billion on prescription drugs, which accounted for nearly 17% of overall personal health care services.
The benefits of pharmaceutical drug therapies are substantial, but these benefits often come with significant financial costs to patients and to payers.
High and rising prices of prescription drugs impact consumers’ access to the medicines they need and their ability to afford other health services and basic necessities.
Fundamental to reducing the escalating cost of prescription drugs is implementing reforms that will lower list prices, increase transparency, and promote competition.
Improve price and quality transparency in the health care system.
The collection and availability of comprehensive health data would allow consumers, policymakers, and experts to have access to health care information, including cost data, to inform consumer decisions and allow for a more robust understanding of the quality and value of health care services in order to reduce health care costs and improve the quality of care.
Critical to driving down health care costs and improving quality is ensuring policymakers and the public have insight into and oversight over underlying prices and quality of health care.
Establish national data-sharing and interoperability standards to reduce waste and improve health care quality.
Establish national data-sharing and interoperability standards to reduce waste and improve health care quality.
National data-sharing and interoperability standards are essential for reducing waste and inefficiencies in the health care system by enabling the real-time coordination of health care services across health care providers and organizations, which will drive needed improvements in the quality and value of health care services.
Ensuring that health care data can flow and is interoperable across the health care system is fundamental to driving improvements in the quality of health care, improving people’s health.
Build a National Health Workforce Designed to Meet the Needs of People and Communities in the 21st Century
Ensuring an adequate workforce is critical to achieving a high-value health care system that meets the needs of the people it serves, including ensuring access to health care services. The current supply, makeup, and distribution of the U.S. health workforce are not adequate to meet the needs of our nation’s families, children, and seniors – including primary care, behavioral health, and oral health needs. Building an adequate health workforce that can meet the needs of all communities is a critical strategy to improve health equity and reduce disparities.
Critical to building a health workforce that meets the needs of people and communities in the 21 is building and implementing a national health workforce strategy focused on building a robust primary care and community-based workforce.
Establish New Economic Incentives to Transform U.S. health care payment and delivery
The health system transformation movement is focused on achieving the triple aim: improving health, improving the quality of care, and reducing health care costs. To achieve the triple aim, the health care system must be re-oriented to deliver health, not just provide health care without consideration for health outcomes. This means that payments to health care providers should be based on keeping patients healthy, and helping them when they become sick, not by doing more tests or procedures to meet an output quota. It also means allowing providers to address the social determinants of health, make improvements in health equity, and keep people healthy by better coordinating services across health care providers, organizations, and social services.
The Impact of COVID-19 on Health System Transformation
As the COVID-19 pandemic sent shockwaves throughout the country, health care providers and organizations worked to respond quickly to provide an effective COVID-19 response. But health care providers who are reliant on fee-for-service payment (FFS) — payments based on the number of services or tests ordered — experienced dramatic and persistent revenue shortfalls as a result of the severe disruption of face-to-face visits caused by the pandemic. These revenue shortfalls threatened the collapse of entire sectors of our health care system, primary care being the most notable example.
- Primary care practices experienced declines of up to 50% in service volume, putting nearly 30% of these practices at risk of going out of business, thereby jeopardizing access to primary care at a time when families needed it more than ever.
- But, providers and health systems participating in efforts to transform their compensation structure to what’s referred to as value-based payment (VBP), have been more financially stable during the pandemic, particularly those who use payment structures that allow providers to receive upfront, ongoing payments not tied to FFS — referred to as alternative payment models.
- Practices receiving these alternative payments were not only able to have a more effective pandemic response but they also were able to build a wide range of capabilities that are not well supported under the current volume-based payment structure of FFS — such as paying for care coordination staff, addressing the social determinants of health, spending more time with patients, patient engagement tools including mobile phone apps and 24/7 helplines, robust data analysis, and infrastructures to support telehealth, remote monitoring, and home-based care.
- Whereas providers who are reliant on the existing FFS payment system have had to rely on Congress and the federal government to make policy changes to have an effective COVID-19 response and to move forward with such innovations.
- COVID-19 has been a stark reminder that we need to transform the way we pay for health care to better support the delivery of high-quality, affordable health care to improve the health of our nation’s families.
The good news is that this transformation is already occurring across the country and there are many examples of health care providers and health systems who are focused on achieving the triple aim. They have changed or are in the process of changing their compensation structures enabling them to provide patients with the specific services that meet their unique health needs. But we need a greater commitment to health system transformation from federal and state policymakers, industry and health systems to scale and spread what is working to achieve health care justice.
key resources

Free COVID-19 Vaccines and Treatments are Here: Why America’s Families Keep Paying
04.15.2021 / Issue Brief






