HOW TO MAKE A HIGH-QUALITY
HEALTH CARE SYSTEM
The good news is that we know where we can make things better, yet federal and state policymakers must have the political will to make real and lasting changes. Community leaders, policymakers, and stakeholders must come together to fill gaps in coverage, ensure access to adequate networks, and make accessible, high-quality, affordable and comprehensive care to all Medicare, Medicaid, and private coverage beneficiaries.
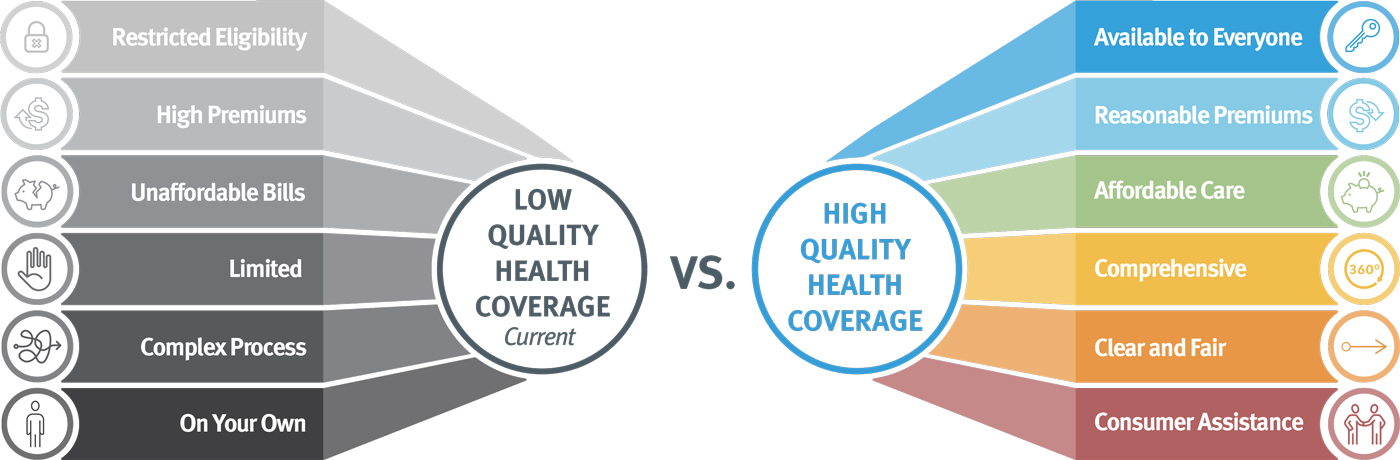
Restricted Eligibility: Qualifying factors for coverage are narrow.
High Premiums: High cost of premiums threatens consumer’s financial security.
Unaffordable Cost-Sharing: Out-of-pocket costs and cost sharing drive up the cost of receiving care.
Limited: The benefits covered under insurance plans are limited.
Complex Process: Navigating the enrollment process is complicated and limits who gains coverage not because of eligibility but because of paperwork
On your own: People are on their own to figure out how to navigate their coverage and challenge unfair bills

Available to Everyone: Coverage is available regardless of income, age, immigration status, location, or employment status
Reasonable Premiums: Premium increases are controlled and there is an affordable premium cost for all consumers.
Affordable Care: The additional costs associated with receiving care are not a limitation to whether someone seeks it out.
Comprehensive: Coverage includes all needed services, and providers, including oral health and mental and behavioral health.
Clear and Fair: The enrollment process is transparent and easy to navigate, in multiple languages. Consumers can determine the difference between plans, make educated decisions about plan choice, and apply for coverage without frustrating and exclusionary processing.
Consumer assistance: Expert help, independent of insurance companies, is available to help consumers navigate coverage and remedy any problems that arise.
 KEY WAYS WE CAN FIX THIS BROKEN SYSTEM
KEY WAYS WE CAN FIX THIS BROKEN SYSTEM
Expand Medicaid as authorized by the ACA in all states.
The Affordable Care Act authorized the expansion of Medicaid in all 50 states. However, only 40 states and the District of Columbia have expanded the program. Medicaid expansion has shown significant benefits including but not limited to: reduced overall mortality, increased access to care for consumers with cancer, disabilities, and chronic conditions, increased rate of insurance for those with diabetes, increased access to postpartum care and better maternal and infant health outcomes, better access to care for rural communities, and increased financial security.
Improve access to Medicaid through smoothing the enrollment processes and expanding eligibility requirements.
The enrollment process, and eligibility requirements for Medicaid can be complicated to navigate and can become a barrier to gaining insurance coverage. Medicaid is required to cover certain populations, such as low-income families, qualified pregnant people, children, and those on Supplemental Security Income. But states can choose to cover more groups such as justice-involved individuals, those receiving community-based services or consumers who are “medically needy”. Expanding the eligibility requirements and the documentation required would allow more American’s to gain access to coverage and Medicaid programs. Additionally, providing adequate timeframes, language assistance, or technical assistance through the enrollment process, or collecting enough data to more seamlessly renew people via the ex parte process would ensure that those who do qualify for Medicaid are not blocked from coverage through technicalities or burdensome paperwork.
Make CHIP, the children’s health insurance program, permanent.
The Children’s Health Insurance Program (CHIP) provides health insurance coverage to children who do not meet Medicaid financial requirements but whose families cannot afford private coverage. CHIP is administered through the states and unlike Medicaid, CHIP is not a permanent program. Congress is required to renew funding for the program. While there have been wins in extending the renewal timeline in recent years, the program that covers millions of children is consistently at risk. Making CHIP permanent, like Medicaid and Medicare, would ensure that this vital insurance coverage does not ever become a pawn of partisan politics and families won’t have to worry about losing health care access for their children.
Maintain robust marketplaces that offer high-quality affordable coverage to individuals.
Health insurance marketplaces play a central role in ensuring that everyone has access to affordable coverage, including families that purchase coverage themselves and those who get coverage through small businesses. The marketplaces offer people choices between different health plans as well as information on cost-sharing and premiums. People can receive premium tax credits that make marketplace plans more affordable based on their income. Marketplaces also can flag eligibility for those who qualify for Medicaid and CHIP. It is essential that robust, competitive, and accurate marketplaces are in place so that consumers can make the best decision about coverage for themselves and their families.
Ensure that premiums and cost-sharing in job-based and individually purchased plans are affordable.
Health care can be expensive even for consumers who have insurance. Premiums, the price that consumers pay for their coverage, and cost-sharing, the amount that consumers pay for covered services (copays, deductibles, coinsurance, etc.), are fees that can add up quickly. Health insurance is meant to make health care more accessible. Ensuring that individually purchased and employer-sponsored health plans are affordable is a baseline for maintaining access to care for millions of consumers.
Ensure health plans have adequate networks and provide comprehensive benefits.
Once a consumer is covered by a health plan, they need to have doctors and other health care providers to go to. Being covered under a health insurance plan gives consumers access to a network of providers, providers and settings where the consumer’s insurance will help shoulder the cost of care provided. Should the network available not have primary care providers, specialty providers, emergency clinics, and more, then the consumer will not have access to care. Federal and state laws require many insurance plans to cover at least a minimum set of essential health benefits, including preventive services, behavioral health, hospital care, pregnancy and newborn care, prescription drugs, and other services, among others. But not all health insurance plans are covered by these laws. Should a plan not provide comprehensive benefits, enrollees may not have access to the care they need to be healthy or to get better.
Provide the assistance needed to obtain, and keep, health insurance.
Understanding how to get coverage and stay covered can be challenging. The eligibility requirements, plan choices, and enrollment processes can be a barrier to accessing insurance coverage for many consumers. Everyone who needs it should have assistance in navigating that process. Assistance can include language or translational assistance, technical assistance to provide documentation and navigate marketplaces, and timely notification of required actions. Once enrolled, people may also need help understanding their benefits and fighting any denials of care. Further, people may lose coverage after a job change, a move, when they age into a different form of coverage, or when they need to recertify. Assisting people to maintain coverage through life and job changes is crucial, it can make the difference to their health stability.
Ensure all health insurance, including Medicare and Medicaid, covers comprehensive oral health services.
Oral health is not a universally required benefit for Medicare, Medicaid, or private insurance plans. Medicare only covers oral health care that is necessary to advance certain medical treatments. Medicaid is not required to provide oral health coverage for adults, and many states do not cover necessary services. Extending oral health services coverage to all insurance plans is an integral part of providing comprehensive coverage. Oral health care can be lifesaving health care for those who struggle to eat, have disabilities, or chronic conditions. Oral health is just as important as other physical health or mental health and is a crucial part of holistic health.
The good news is that there has been a ton of progress across the country, on both the state and federal level. We have seen expansion of Medicaid and marketplace coverage and movement towards coverage of a more comprehensive set of services. We need to defend these advances while continuing to improve access to high-quality coverage.




