We want to provide the best care possible to our patients without worrying if we can keep the lights on.
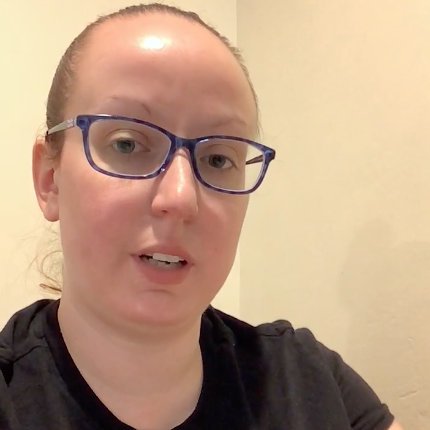
Katherine Twomey, a licensed clinical social worker and lifelong Long Islander, has dedicated her entire career to community mental health. Living in New York’s 1st Congressional District, she works as a psychotherapist at a community mental health clinic where she and her colleagues serve patients with severe mental illnesses such as schizophrenia and schizoaffective disorder. Nearly all of their patients rely on Medicaid.
Now, with HR1 officially passed and Republican health care cuts signed into law, Twomey faces the reality of its impending consequences. The sweeping Medicaid cuts outlined in the legislation threaten not only the future of the clinic but the well-being and survival of the patients it serves.
“The Medicaid cuts contained in the Big Beautiful Bill will be devastating for our patients and for clinics like mine,” Twomey said. “Despite reassurances that these cuts will not harm disabled people, there is no way to implement them without causing direct harm to people, including those with disabilities.”
Many of her patients live with psychiatric conditions that prevent them from working in any capacity. Yet their applications for Social Security Disability Insurance (SSDI) are frequently denied. “It can take years for an appeals process with the Social Security Administration to yield any results,” she explained. “Despite their significant psychiatric disabilities, the government deems them fit to work.”
Those same patients will now face strict work reporting requirements to keep their Medicaid coverage. Twomey and her fellow providers must complete burdensome paperwork just to exempt patients from these requirements, further straining clinics that are already stretched thin. “We are already at capacity with direct patient care and this bill places an increased administrative burden upon us,” she said.
The law also changes how clinics like hers can bill Medicaid retroactively. Until now, they had a 90-day window to file for retroactive billing, a policy that made it possible to begin treating patients immediately while ensuring the clinic remained financially viable. Under the new law, that window shrinks to just 30 days. “The one big beautiful bill will limit us to just 30 days of retroactive billing, making it more difficult for patients to access care and for providers to grant care.”
For patients already navigating complex mental health conditions, any disruption in care could be catastrophic. “These include relapsing symptoms, inpatient hospitalizations, and a heightened risk of suicide attempts and completed suicides,” Twomey warned. “Their lives depend on a robust and accessible Medicaid program.”
As the law’s provisions move toward implementation, Twomey urges policymakers to recognize the stakes. “We want to provide the best care possible to our patients without worrying if we can keep the lights on,” she said. “Our patients want to receive the best care possible without worrying if they can afford it.”
With the health and safety of vulnerable individuals at risk, Twomey calls on Congress to urgently “protect health care for all people.”
Add your voice to help us continue to push for the best health and health care for all.
SHARE YOUR STORY