
Why States Should Suspend Medicaid for People During Incarceration
03.08.2016
With a majority of states expanding Medicaid, many more people stand to gain health coverage, including those recently released from jail or prison. States are re-evaluating their policies regarding Medicaid for incarcerated residents.
We’ve taken a closer look at what states have accomplished so far to get a better idea of how this has played out across states. We found that 34 states and the District of Columbia now have some form of policy to suspend Medicaid for people in prison or jail. Here, we explain why more states should adopt this policy.
Why health coverage matters for people leaving incarceration
We all have a stake in ensuring that people recently released from incarceration can get health coverage without jumping through administrative hoops or waiting several months to get back into the health care system. Access to health care has proven crucial to helping people avoid returning to jail or prison after release.
People re-entering communities following incarceration have significant health care needs, yet many are uninsured, and therefore go without needed care. The expansion of Medicaid under the Affordable Care Act (ACA) presents states with new options for extending health coverage to this population. Those who could benefit include people on parole or probation, serving short terms in county or state jails, and serving longer sentences in state or federal prisons.
States can choose to terminate or suspend Medicaid during incarceration
People in the criminal justice system are not able to use Medicaid while incarcerated (unless it’s for inpatient services). However, as our new 50-state map shows, when an individual leaves incarceration, the process for handling his or her Medicaid varies widely by state.
States have two options when someone is incarcerated:
- Terminating the individual’s Medicaid: In states that terminate someone’s Medicaid eligibility, he or she must re-apply and re-enroll upon release from jail or prison. In addition to making it harder for the individual to obtain needed health care, termination creates an administrative burden, requiring the state to process a new application and check the person’s eligibility again.
- Temporarily suspending the individual’s Medicaid: In states that suspend Medicaid eligibility, coverage can be reinstated more quickly. States can either suspend Medicaid for the duration of an individual’s incarceration or suspend it for a specific length of time (such as 30 days). Time-limited suspension is helpful for people with short periods of incarceration, but it requires those with longer stays to re-apply for Medicaid upon release. Currently, 16 states follow a time-limited suspension policy. States also have the option to suspend Medicaid for those serving time at certain institutions (for example, a state may suspend Medicaid for those in county jails but not suspend for those in state prisons).
Termination of coverage can often lead to gaps or lapses in health care coverage. Suspension of Medicaid gives those re-entering their community a more seamless path to coverage. Not only is this easier on the individual, but it is also a much more efficient process for the state Medicaid agency. Plus, if the state suspends Medicaid, its Medicaid agency can reimburse jails and prisons for inpatient hospital services that people receive during their incarceration.
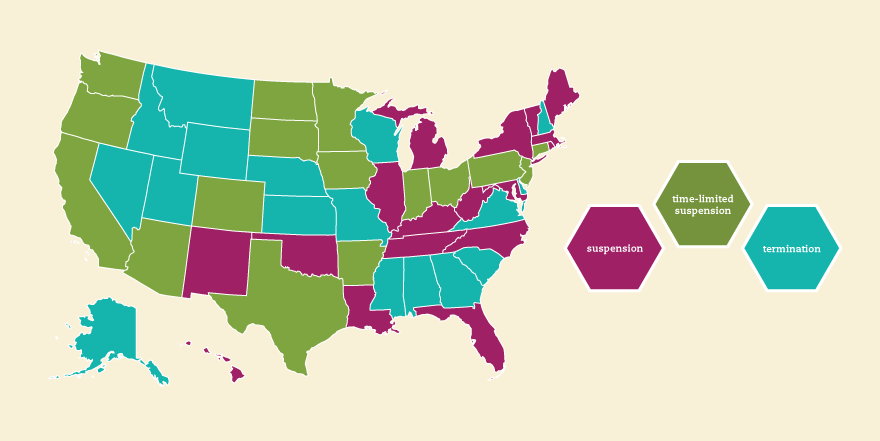
Our new 50-state map shows which states suspend and which states terminate Medicaid for people entering jail or prison.
Changing a state’s Medicaid suspension policy is a multistep process
While the Centers for Medicare and Medicaid Services (CMS) recommends that states suspend Medicaid, states ultimately retain flexibility regarding how they make that transition.
To suspend Medicaid during incarceration, a state must take multiple steps to implement the policy change. The processes differ by state, and it’s important to know the steps required in your state when beginning to engage in this work.
Of the 34 states that now have some form of suspension in place, some states passed legislation to do so. These include California, Florida, and New Mexico. Other states, such as New Jersey and North Carolina, used an administrative process to switch policies.
Why now? The option to suspend Medicaid has existed for some time. Many states didn’t adopt this option before, however, because so few people were eligible for coverage before the ACA’s expansion of Medicaid.
Making the case to suspend Medicaid instead of terminating coverage
If you’re interested in working with your state to suspend Medicaid for incarcerated residents, consider finding partners that have a similar interest in making continuous health coverage available to people leaving prison or jail. You may find allies in jails, social services agencies, workforce development programs, community health centers, consumer advocacy organizations, and in-person assister organizations.
When working with these partners, focus on these key points that are most likely to resonate with policymakers:
- Evidence shows that access to health care can prevent individuals from cycling in and out of the prison system. This leads to savings for both state and local jails and prisons, especially because the vast majority of individuals spending time in a correctional facility are arrested again.
- Suspending eligibility allows states to obtain federal Medicaid fundingfor inpatient services for individuals who are currently incarcerated. This allows states to save on costs of care for by tapping into federal dollars. If someone is newly eligible for Medicaid, the state will receive an enhanced federal match for his or her coverage.
- Suspending Medicaid creates less administrative work for the state because the Medicaid agency will not have to process new applications. Instead, the state will only restart an individual’s existing coverage.
- When people involved in the criminal justice system have health coverage and can obtain care, they are more likely to experience a seamless re-entry, be more equipped to hold stable jobs, and be productive members of society.
- Connecting people to coverage reduces uncompensated care. When people have health coverage, they are less likely to have costly visits to the emergency room and more likely to receive preventive services.
Policies around this issue are changing fast, and we’re eager to see more states adopt the policy change to suspend Medicaid for incarcerated individuals. If you’d like guidance about how to get involved in this work, email us at assisters@FamiliesUSA.org.
Listen to a webinar Families USA hosted on best practices for outreach and enrollment for incarcerated residents.




