
Tackling Health Disparities While Reforming Payment and Delivery
05.05.2015
In part 1 of this blog series, we explained that efforts to reform health care delivery and payment methods could be a double-edged sword for communities of color and described one example of a sustainable intervention that tackles health disparities. In part 2 we review innovative models currently in place in New Jersey and New Mexico.
The activity around payment and system reform creates an opportunity to develop interventions that directly address racial and ethnic health disparities. However, some reforms could inadvertently make disparities worse. For example, they could discourage providers from treating sicker, more complex patients, or undermine the financial viability of struggling safety net providers.
Fortunately, some communities are implementing delivery system reforms that reduce health disparities and bend the cost curve. The effective models we describe in this blog series share several features in common. They all:
- are designed for the community being served
- improve care for specific populations
- reduce spending—and have become sustainable and replicable by tapping into Medicaid as a funding source.
In part 1 last month, we described Minnesota’s successful Medicaid Community Health Worker model. Here we highlight models from New Jersey and New Mexico.
New Jersey: “Hot-spotting” targets services to the most vulnerable, high-utilizing patients to improve health care access and quality, reduce disparities, and lower costs
The use of “hot-spotting” in Camden, New Jersey, is revolutionizing care for patients who frequently utilize high-cost services while reducing overall costs for the system. Crystal McDonald, director of organizing at Faith in New Jersey, described the model during a workshop at Health Action 2015. Among other activities, McDonald’s group partners with communities, doctors, and other service providers to make the hot-spotting model work.
In Camden, just 1 percent of patients drove 30 percent of hospital expenses
With hot-spotting, providers use hospital admissions data and census-tract mapping to identify and target services to high-need patients whose care drives a disproportionate share of health care costs. Th Dr. Jeffrey Brenner of the Camden Coalition of Healthcare Providers (CCHP) developed the hot-spotting model. In Camden, just 1 percent of patients drove 30 percent of hospital expenses, costing more than $30 million per year. Known as “super utilizers,” these patients:
- suffered from chronic diseases
- often struggled with complex social challenges and mental illness
- were primarily low-income African Americans
- were geographically concentrated in certain areas
As a result of these barriers to care, patients utilized poorly coordinated, more expensive services. CCHP partnered with a local faith-based organization, Camden Churches Organized for People, an affiliate of Faith in New Jersey, to talk with the community in these hot spots about the services and supports they needed to improve their health. Along with medical and social service providers, they developed community-focused, geographically targeted approaches to address these barriers to care.
Multidisciplinary teams reached out to give patients additional health care support
For example, outreach teams of social workers, medical assistants, and nurse practitioners connected patients with primary care homes. They also provided patients with the supports they needed to access care and adhere to their care plans. As a result, more patients received the right care at the right time to manage their chronic conditions, which significantly reduced hospital admissions—improving patients’ health while reducing spending.
Despite CCHP’s well-documented success, finding consistent funding for hot-spotting remains a challenge. Provider groups and health systems across the country that are replicating this model rely largely on private funders, like the Robert Wood Johnson Foundation. In Camden, however, stakeholders succeeded in getting the program funded under Medicaid through an Accountable Care Organization pilot, which began this past year.
New Mexico: Reducing disparities with a health care payment model that combines hot-spotting and community health workers to improve outcomes and reduce costs.
New Mexico is experimenting with a novel payment and delivery model that combines hot-spotting principles with the strategic use of community health workers (CHW). Charlie Alfero, of Hidalgo Medical Services Center for Medical Innovation, explained how this model allows CHWs to work on three different levels:
- provide intensive services for super utilizer patients with the highest need
- support patients in managing their chronic diseases, and
- provide community level health promotion, such as health education and preventive services, for Medicaid managed care enrollees.
This model sets up two funding streams for CHW services based on patient need that are independent from medical care payments. It was developed as a collaboration between the University of New Mexico, Molina Healthcare (a Medicaid managed care plan), and Hidalgo Medical Center, a federally qualified health center that serves a majority Latino population.
Level of CHW services provided is based on intensity of patient’s need
As illustrated in the graphic below, the patient population is stratified into three levels based on care utilization and health status. High utilizers, the top 5 percent that generate 50 percent of health care costs, are categorized as Level 3. The next highest 15 percent, that generate 30 percent of health care costs, are designated as Level 2, and the rest are Level 1.
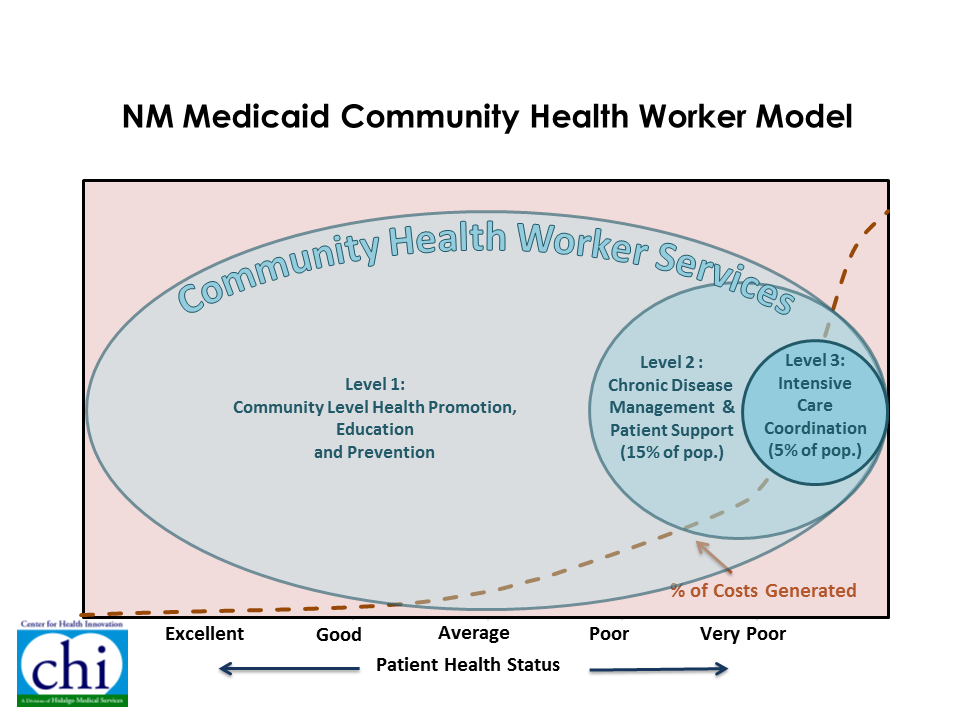
For Level 3 patients, CHWs provided intensive care coordination, chronic disease management (CDM) and individual patient support, for which the provider is paid roughly $300 dollars per member per month (PMPM). CHWs provide Level 2 patients with CDM and patient support. All the enrollees benefit from the services CHW’s provide. These include community-level health promotion, education, and prevention activities. Hidalgo receives $6 PMPM for Level 1 and 2 patients.
Extra support for the sickest patients improves outcomes, generating savings that can be reinvested in improving community health
The first phase of this project, focusing exclusively on the highest-need patients, was so successful in improving access, reducing utilization, and improving patient health that Molina saved $4 for every Medicaid dollar spent.
The separate funding streams allow CHWs to address health inequities on several different levels, enabling them to spend the time necessary to help a few very sick patients, but also to spend time doing community-wide, preventive care activities. This model will be fully implemented in locations across the state for Molina and Blue Cross Blue Shield Medicaid managed care enrollees by July of this year.
Models offer path forward for reforms that reduce ethnic and racial health disparities
Racial and ethnic health disparities are pervasive and must be eliminated to ensure a healthy country, productive workforce, and sustainable health care system. We must transform our health care payment and delivery system to achieve this goal, but focusing primarily on cutting costs could unintentionally increase health disparities. Minnesota, New Jersey, and New Mexico show that reforms that tackle disparities head on can reduce costs by improving quality. Advocates and policy makers should build these kinds of reforms into health system transformation efforts to reduce health disparities and improve health care not only in communities of color, but for everyone.
