
Recent Hospital Earnings Data Show Stark Contrast in Numbers of Uninsured Patients in Medicaid Expansion States Compared to Non-Expansion States
05.27.2014
There is now more proof that hospitals have an enormous financial stake in state decisions about expanding health coverage to low-income families.
Since the passage of the Affordable Care Act, about half the states have chosen to expand health coverage to low-income families, taking advantage of federal matching funds to pay for a Medicaid expansion. This expansion has provided health insurance and financial security to millions of people while also injecting needed federal dollars into local economies. But for the states that have rejected the option to expand health coverage, the economic consequences are wide-ranging. Nowhere is this more evident than in hospital rooms across the country.
A few weeks ago, Jason Millman reported in The Washington Post’s “Wonkblog” that publicly traded hospitals are noticing a big difference in the insurance status of the patients that they are seeing in Medicaid expansion states compared to patients in states that have not expanded Medicaid.
In Medicaid expansion states, hospitals report admitting more patients who have health insurance that is covered by Medicaid—while simultaneously seeing a drop in the number of uninsured patients. That’s good news for hospitals, because it means that more of the patients they are caring for have insurance to cover their medical bills.
And as USA Today pointed out on Saturday, safety net hospitals—typically government-owned or nonprofit hospitals that disproportionately serve the poor—are also seeing a drop in uninsured patients.
But in non-expansion states, hospitals report treating slightly higher numbers of uninsured patients—along with a drop in patients who are covered by Medicaid. For these hospitals, that means that they have more patients who cannot pay their bills, a consequence that has been shown to affect both a hospital’s bottom line and the cost of insurance for everyone else.
Case study: The Hospital Corporation of America (HCA) reveals stark contrasts in rates of uninsurance
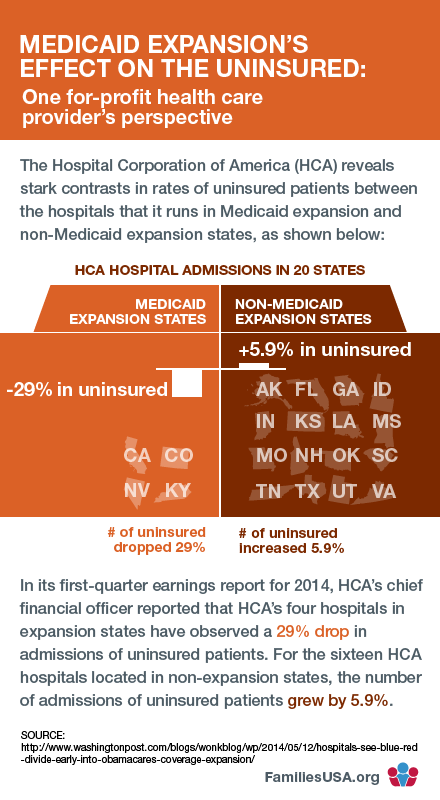
The Hospital Corporation of America (HCA) operates hospitals in 20 states, four of which have expanded Medicaid and 16 of which have not.
As Millman notes in his article, the HCA chief financial officer reported that its hospitals in expansion states have observed a 29 percent decline in admissions of uninsured patients and a 22 percent increase in admissions of patients covered by Medicaid.
But for HCA hospitals located in non-expansion states, the number of admissions of uninsured patients grew by 5.9 percent. Community Health Systems and Tenet Healthcare have seen similar results.
Keep in mind that Millman is reporting on earnings calls from publicly traded hospitals. We don’t yet know what is happening at public hospitals, privately owned hospitals, or not-for-profit charity hospitals.
The cost of treating uninsured patients raises health insurance premiums for everyone
The growth in admissions of uninsured patients is troubling: It’s not just bad news for a hospital’s bottom line—it’s bad news for the rest of us, too.
Hospitals treat all patients, whether they have insurance or not. But when a patient is uninsured, the hospital has to make up for the cost of treating that patient. In a hospital’s budget, this cost is called “uncompensated care,” and those costs get passed on to patients who do have insurance. Our earlier research on uncompensated care found that hospitals, doctors, and other health care professionals provided $42.7 billion in uncompensated care in 2008. Health insurers passed these costs on to families and businesses in the form of higher health insurance premiums.
Putting politics aside: Medicaid expansion is a boost for state economies
Medicaid expansion is not just good for patients—it’s good for state economies, too. For example, The Lewin Group estimated $101 billion in net savings to states would come from the Medicaid expansion between 2014 and 2019.
States can choose to expand Medicaid at any time. In states that haven’t yet made that choice, these data from hospitals are one more reason that state leaders should put politics aside and take steps to expand Medicaid in their states.
This article was written with the assistance of Shannon Donahue, Deputy Director of Government Affairs.
