Dental Therapists Can Improve Access to Dental Care for Underserved Communities
By Lydia Mitts, Sinsi Hernández-Cancio,
11.28.2016
Millions of people in this country face significant barriers to obtaining the basic dental care they need to achieve good oral health. As a result, more than half of people in the U.S. go without any dental care each year, and many struggle with untreated dental disease that can have far-reaching, serious effects on their overall health.
Untreated dental disease can have serious consequences for people’s health. One reason some people can’t get access to timely dental care is the shortage of dental providers in many areas. These shortages hit some communities especially hard, particularly rural areas, and low-income neighborhoods, where people of color are more likely to live.
Adding dental therapists to the dental workforce is an important step states can take to improve access to dental care in underserved communities.
This burden of untreated dental disease disproportionately falls on communities of color, who already struggle with other serious health inequities, some of which could potentially be exacerbated by poor oral health.
In addition, unmet dental care needs exact an avoidable cost on the health care system each year as millions of dollars are spent on preventable dental-related emergency care each year.
People in the United States face many, often interrelated barriers to getting access to the dental care they need when they need it. For many, one serious obstacle to care is the fact that there aren’t enough dental providers near where they live. In fact, the Health Resources and Services Administration (HRSA) has identified nearly 5,000 dental provider shortage areas across the country (areas where there aren’t enough dentists to meet the needs of the community).
Shortage areas affect communities of all incomes, all racial and ethnic backgrounds, and all levels of urbanization. However, they are most common in rural areas and lower-income neighborhoods.
Communities of color are especially affected by dental provider shortages. On average, they are more likely to live in low-income areas where provider shortages are more likely to exist. Layered on top of this, certain racial and ethnic minorities are vastly underrepresented in the dental workforce. While black non-Hispanics, Hispanics, and American Indian/Alaska Natives together make up 32 percent of the U.S. population, they account for barely 10 percent of dentists in this country. This makes it incredibly challenging for these communities of color to access care from providers who are best suited to meet their cultural and linguistic needs.
Dental therapists are part of a dentist-led team. They educate patients about oral health and prevention, perform dental evaluations, give fluoride treatments, place sealants, clean teeth, place fillings and perform simple extractions.
Like nurse practitioners and physicians assistants in the field of medicine, dental therapists expand the reach of dentists and free them to perform more advanced treatments.
Expanding and diversifying the dental workforce to meet the needs of all communities is a critical component to improving access to timely, culturally competent care and to addressing health disparities. Addressing dental workforce shortages and improving timely access to dental care can also improve the overall quality and cost-effectiveness of care.
Adding dental therapists to the dental workforce is one strategy that states should use to improve access to timely dental care and to diversify the dental workforce to better meet their communities’ needs. States that want to expand their dental workforce to include dental therapists must pass legislation that authorizes dental therapists to practice in their state and determine the scope of practice for these providers.
What’s the problem?
Dental Provider Shortages Are a Major Barrier to Obtaining Timely Care
For many people, a major barrier to getting timely dental care is that there aren’t enough appropriate providers to go around. Nearly 49 million people live in oral health professional shortage areas. Shortage areas are most common in rural areas and in low-income communities, where people of color are more likely to live.
In the United States, dental provider shortages are only one of many interrelated factors that prevent people from getting the dental care they need to maintain good oral health. Not having comprehensive dental coverage and being unable to afford the cost of dental care are other major impediments to getting access to care.
Even when people do have dental insurance, they might not be able to find a provider in their network who is taking new patients.
In addition, there are multiple broader socio-economic barriers to obtaining dental care including lack of transportation, not having sick leave, limited understanding of how our health system works, low health literacy, and distrust of the system and of providers based on prior negative experiences or discrimination.
In addition, there are even fewer dentists who accept Medicaid. A 2010 study found that fewer than half of the dentists in 25 states accepted any Medicaid patients at all. This can make getting access to dental care particularly difficult for people on Medicaid, even outside of shortage areas. In 2014, on average, more than half of children across all states’ Medicaid and CHIP programs went without any preventive dental care. The shortage of dentists who accept Medicaid is a particular problem for low-income communities and people of color, who are more likely to rely on Medicaid to get the care they need.
Dental Care Disparities are Particularly Acute in Communities of Color.
The immense disparities in access to dental care across the country disproportionately affect racial and ethnic minorities. In particular, non-Hispanic blacks, Hispanics, and American Indians and Alaskan natives have the poorest oral health of the racial and ethnic groups in this country.
Among adults ages 20-64: Hispanics are 50 percent more likely to have untreated tooth decay than non-Hispanic whites; Non-Hispanic black adults are two times as likely to have untreated tooth decay as non-Hispanic whites. Non-Hispanic blacks and Hispanic adults are also nearly 50 percent more likely to have gum disease than non-Hispanic white adults.
» Non-Hispanic black and Hispanic adults are significantly more likely to go without any dental care in a year compared with nonHispanic white adults.
» Non-Hispanic black and Hispanic children ages 2 to 8 are twice as likely to have untreated tooth decay as non-Hispanic white children.
» American Indian and Alaska Native children ages 3 to 5 are four times more likely to have untreated tooth decay as white non-Hispanic children.
Dental Provider Shortages in Communities of Color are Exacerbated by Limited Provider Diversity
For care to be truly accessible, high-quality, and patient-centered, it must meet people’s cultural and linguistic needs and be grounded in an understanding of the communities in which they live.
Many communities of color face added difficulty getting access to care from providers who are equipped to provide culturally competent care. If there are too few dentists to go around, there are even fewer dentists of certain racial and ethnic minorities. Non-Hispanic blacks, Hispanics, and American Indian/Alaskan Natives make up barely 10 percent of dentists, but more than 30 percent of the population. Further, only 8 percent of students in training to become dentists are black, Latino, or American Indian.
For care to be truly accessible, high-quality, and patient-centered, it must meet people’s cultural and linguistic needs and be grounded in an understanding of the communities in which they live. To be sure, providers don’t necessarily have to come from the same racial and ethnic background to provide high quality, culturally competent care, but sharing common experiences and language can help tremendously in reducing more intangible (but no less important) barriers to high quality care. These barriers include confusion about the health care system, cultural differences that interfere with communication, trust, and previous experiences of being treated with disrespect and even racism.
Diversifying the dental workforce is essential to improving people of color’s access to high-quality dental care. Not only are providers of color usually better able to provide culturally competent care to people of color, they are also more likely to choose to work in minority and underserved communities.
Improving cultural competency of care in this country is of paramount importance to improving the quality of care and health outcomes that our system delivers.
Emergency Rooms Are the Only Available Source of Dental Care for Some
The emergency room can be the only accessible source for dental treatment for people who struggle to get access to timely care. This means that many people are only able to obtain care once they face painful complications that could have been prevented if they had access to basic care. In 2009, more than 800,000 visits to the emergency room were related to preventable dental conditions.
These emergency room visits come at an immense cost to states and other health care payers: It is estimated that the average cost to Medicaid for inpatient emergency treatment of dental problems (for patients admitted to the hospital from the emergency room) is almost 10 times more than the cost of providing preventive dental care. The cost of outpatient emergency room care is nearly three times more than the cost of preventive care.
Improving access to timely, preventive dental care and routine treatment in more cost-effective outpatient settings is critical to preventing more serious dental problems. It also helps improve communities’ overall oral health. This, in turn, can help reduce the need for dental-related emergency room visits and the corresponding costs to the health care system.
Unmet Dental Care Needs Can Contribute to Other Health Disparities
Untreated dental disease can have far-reaching consequences for people’s overall health and wellbeing. Without access to necessary care, dental infections can spread throughout the body and affect other areas of people’s health. Growing research has found that untreated dental conditions can put people at greater risk for other health concerns. These include conditions where there are already significant racial and ethnic health disparities.
Diabetes is a prime example. Racial and ethnic minorities are more likely to have diabetes and are at increased risk for complications from diabetes, such as blindness and kidney disease. While there are a number of factors that contribute to these disparate outcomes, there is growing clinical evidence that shows access to dental care may be one piece of this puzzle. There is strong evidence that untreated gum disease can raise blood sugar levels, and, in turn, increase the risk of related complications. In addition, people with diabetes who are unable to meet their blood sugar targets are at increased risk of developing the very gum disease that can place them at higher risk for further diabetes complications.
Timely dental care is therefore one of a number of types of care and resources that patients need to effectively manage their diabetes. Recent studies have found that treating gum disease in diabetic patients can actually help improve their diabetes management outcomes.
Premature birth is another example of a health issue where there are significant racial and ethnic disparities and where access to dental care could make a difference. Non-Hispanic black women have significantly higher rates of preterm birth compared to non-Hispanic white women. And preterm birth is the leading cause of death for black infants, who are twice as likely to die before their first birthday as non-Hispanic white babies.
A growing body of research suggests that untreated gum disease is one of many factors that can increase a woman’s risk of giving birth prematurely.
Given the growing evidence that dental disease can have a far-reaching impact on other clinical conditions, it is important to consider how disparities in access to dental care may contribute to disparities in other clinical areas.
A Strategy That Addresses This Problem: Adding Dental Therapists to the Workforce
Why States Are Considering Adding Dental Therapists to their Workforce
As states, advocates, and community leaders work to improve the value of health care and address broader health disparities, these efforts must include strategies to reduce disparities in access to timely dental care for communities of color.
To improve access to dental care for communities of color and other underserved communities, states must develop strategies to expand the dental workforce and increase the capacity of dental practices to serve more people in these communities. One option for achieving this goal is for states to pass legislation that grants licensing to mid-level dental providers, called dental therapists, to provide care.
Dental therapists work as additional members of a dentist-led team. They provide health education; preventive care (including sealants that protect teeth from cavities); and limited, non-surgical restorative dental services, such as fillings, crowns, and tooth extractions. Each state determines the full scope of services that dental therapists are allowed to provide through “scope of practice” laws and regulations.
Dental therapists are not a new type of provider. More than 50 countries have thriving dental therapy programs that have been shown to improve access to high-quality care. In the United States, there are a growing number of places in which activity is underway to bring dental therapists into the oral health workforce.
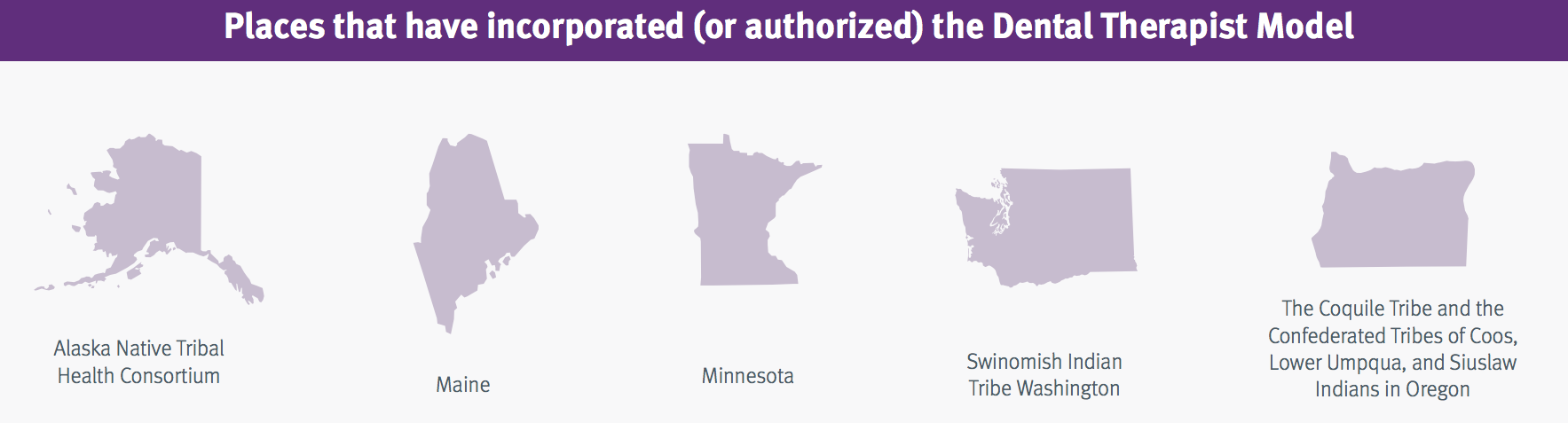
» In Indian country, a growing number of tribes and Indian health boards are employing dental therapists to serve their American Indian/Alaskan Native communities. In 2003, the Alaska Native Tribal Health Consortium created a Dental Health Aide Therapist (DHAT) Initiative, which added dental therapists to the care teams serving Alaska native villages state-wide. The Swinomish tribe in Washington began employing dental therapists in early 2016. In 2016, The Coquile Tribe and the Confederated Tribes of Coos, Lower Umpqua, and Siuslaw Indians in Oregon also received approval for a pilot project to employ dental therapists under a state initiative aimed at expanding innovations in oral health care.
» In Minnesota, dental therapists have been providing care since 2011.
» Maine and Vermont have passed legislation to allow dental therapists to practice.
Close to a dozen additional states are currently considering legislation to allow mid-level dental providers to practice.
What training do dental therapists receive?
For people who want to become dental health providers, dental therapy training is a new, more accessible career path compared to becoming a dentist.
Typically, dental therapists complete two to three years of hands-on competency-based training from a post-secondary dental therapy education program. In many ways, their training parallels the training that dentists receive, but dental therapists are trained to perform a narrower scope of procedures than dentists. New national accreditation standards for dental therapist training programs are in the process of being implemented, which will allow existing and future training programs to seek accreditation.
For people who want to become dental health providers, dental therapy training is a new, more accessible career path compared to becoming a dentist. Dental therapy training is a college program rather than a doctoral program. It takes less time and money to complete than going through four years of college and then four years of dental school. These factors make it a faster, more accessible, and affordable process to become a dental care provider. As such, dental therapist programs can create opportunities for people from more diverse backgrounds and communities to enter the dental care workforce, especially for people from underserved, low-income communities.
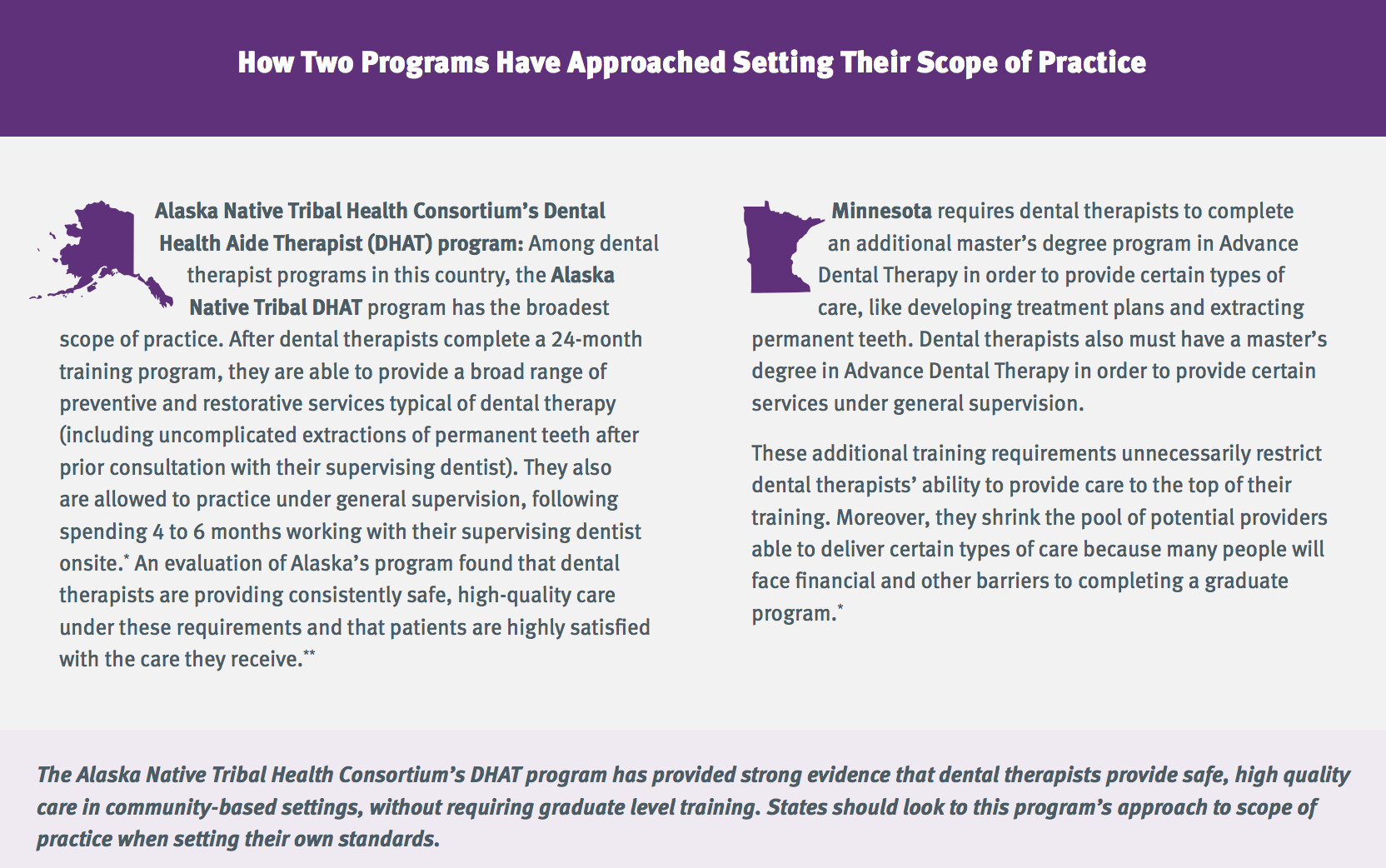
States are responsible for setting the training requirements for dental therapists, as part of the scope of practice laws and regulations. States should avoid any standards that would require dental therapists to have a masters degree in order to perform services that they are well trained to perform under a competency-based post-secondary program. Adding additional training requirements can make advancing in the workforce less accessible to individuals who face barriers to pursuing graduate level training. It also can limit dental therapists’ ability to provide communities with the highest level of care they are trained to deliver.
How are dental therapists supervised by dentists?
States decide how dentists supervise dental therapists under scope of practice laws and regulations. The options range from requiring dental therapists to work in the same site as a supervising dentist to allowing dental therapists to practice at a different site and remotely consult with their supervising dentist—what is known as “general supervision.” Under general supervision, the supervising dentist and dental therapist agree on the scope of services that the dental therapist will provide off-site.
To maximize the positive impact that dental therapists can have in communities, it is critical that states allow dental therapists to provide care under general supervision. This approach is safe and offers immense benefits to communities: It allows dental therapists to expand the reach of a dental practice into community-based settings that may be more accessible to underserved populations, such as remote dental clinics and schools.
States should avoid restrictions that require dental therapists to only provide care onsite with a dentist. This can prevent them from serving hard-to reach, remote populations and can handicap their ability to improve access to dental care in local communities.
Why Scope of Practice Requirements Matter: Lessons Learned from Two Programs
States determine the scope of services that dental therapists are allowed to provide, the minimum training requirements for providing those services, and the supervision requirements. To best meet the needs of underserved areas, policymakers need to set requirements that allow dental therapists to deliver the highest level of care they are trained to provide in local community-based settings.
What do good scope of practice requirements look like?
In order to achieve these aims, states should allow dental therapists to deliver the full range of care that they have been shown to safely deliver through postsecondary, competency-based training.
States should also allow dental therapists to provide care under general supervision, which enables them to extend the reach of a dental practice to more accessible community-based settings.
The experience of the Alaska Native Tribal Health Consortium’s Dental Health Aide Therapist (DHAT) program exemplifies the positive impact of setting standards with these elements. In contrast, the standards in Minnesota’s dental therapist program demonstrate the limitations of adding unnecessary restrictive standards.
Why is the dental therapist model good policy?
Dental Therapists Expand Access in Underserved Areas
Evaluations have found that dental therapists provide high-quality, patient-centered care to underserved areas and improve access to preventive care.
Since the Alaska Native Tribal Health Consortium’s DHAT program started, dental therapists have extended care to 45,000 previously underserved people.
In Minnesota, state law requires that dental therapists practice in settings that primarily serve low-income or underserved communities. In clinics that employ dental therapists, on average, more than 80 percent of the patients treated by dental therapists have been people with public insurance, like Medicaid. The state has also seen a decrease in patients reporting long wait times and travel times for dental care.
Adding Dental Therapists Can Help Diversify the Dental Workforce
Dental therapy programs are a good way to create opportunities for people from more diverse socioeconomic and racial and ethnic backgrounds to enter the dental workforce. The shorter, more affordable process to become a dental therapist will enable people for whom dental school is out of reach to get the training they need to serve their communities.
The Alaska Native Tribal Health Consortium’s DHAT program has been especially effective in training therapists from within the Alaska native community. Nearly 90 percent of dental therapists practicing in Alaska native communities are Alaska native or American Indian, and many returned to their home village to provide care after they completed their training. As members of the communities they serve, they are better equipped to provide culturally competent care, and they are seen as role models.
Dental Therapists Can Help Reduce Dental Emergencies
There are early signs that using dental therapists to provide preventive care is helping reduce the amount of emergency dental problems and the use of emergency rooms for dental care. In both Alaska and Minnesota, the majority of care provided by dental therapists has been preventive and diagnostic care.
One clinic in Alaska has documented a shift in the kind of dental services it provides since it began employing dental therapists.
» In 2009, emergency services were the most common type of care the clinic provided, accounting for close to 40 percent of its care overall.
» By 2014, preventive care was the most common type of care provided, and emergency care had declined to less than 25 percent of the services provided.
This is a hopeful sign that improved access to preventive care is actually reducing the incidence of more serious and more costly problems.
In Minnesota, two provider systems have placed dental therapists in hospital-based clinics to serve patients who otherwise would have been treated in the emergency room.
Dental Therapists Are a Cost-Effective Way to Expand Access to Care
Adding dental therapists to a state’s dental workforce is an affordable approach to strengthen the workforce and help address unmet dental care needs. Salaries of dental therapists are lower than that of dentists, making them a less costly way to expand a dental practice’s staff capacity. Not only do dental therapists enable practices to see more patients, they allow dentists to devote more of their time to providing more complex care. Multiple evaluations have found that employing dental therapists is cost-effective for dental practices. One study found that the revenue generated by hiring dental therapists is more than triple that of their salaries.
More broadly, adding dental therapists to the workforce is a budget-friendly way for state and local dental workforce investment programs to diversify and expand the workforce. Grants and scholarship funds can help train more dental professionals in a shorter period of time if a portion of those funds is dedicated to training dental therapists. This enables these programs to more rapidly expand the dental workforce within their current budgets.
Next Steps for Advocates
In a number of states, advocacy efforts are underway to add dental therapists to the dental workforce. This requires passing legislation that authorizes dental therapists to be licensed as providers, as well as establishing a defined scope of practice for these professionals through either legislation or additional regulations.
Policy Recommendations for Legislation
To maximize dental therapists’ ability to improve access to care in underserved areas, state legislation should:
» Permit dental therapists to work under the general supervision of a dentist in communitybased settings.
» Establish a scope of practice that allows dental therapists to provide the full range of care that they have been shown to competently deliver.
» Require dental therapists to provide care in underserved communities and in dental provider shortage areas.
Advocacy Strategies

To advance legislation that allows dental therapists to practice in a state, communities should demonstrate a need for expanded dental teams that include dental therapists. They should also develop networks of key supporters. Successful strategies include these steps:
» Documenting the unmet dental needs of communities by pairing federal data that maps dental provider shortage areas with the personal stories of community members who have trouble getting the care they need.
» Gathering data on what the state spends on dentalrelated emergency room visits, and, if possible, the related uncompensated care costs for hospitals. A state’s department of public health or Medicaid office could be helpful resources in identifying data.
» Engaging affected communities at the state and local levels, including health equity and racial justice leaders. This is critical to ensuring that the policy solutions that are developed are driven by—and meet the needs of—those communities.
» Building diverse stakeholder allies, including dentists, to help champion legislation. At both the state and national levels, dental associations have been outspoken in their opposition to allowing dental therapists to practice. Finding individual dentists who are vocal supporters of dental therapists will be important to countering this opposition.
» Considering “strange bedfellow” allies: In some states, advocates for free market policies have been key allies in advancing the use of dental therapists because they see it as a market-driven solution for improving access to care.
Addressing problems in getting access to dental care is critical to state efforts to improve residents’ health, lower health care costs, improve health care quality, and reduce racial and ethnic health disparities. Adding dental therapists to a state’s dental workforce is a cost-effective strategy for achieving these goals. Dental therapists provide high-quality, patient-centered care and improve access to routine care in low-income and rural communities, including communities of color.